| Korean Med Educ Rev > Volume 26(Suppl1); 2024 > Article |
|
Abstract
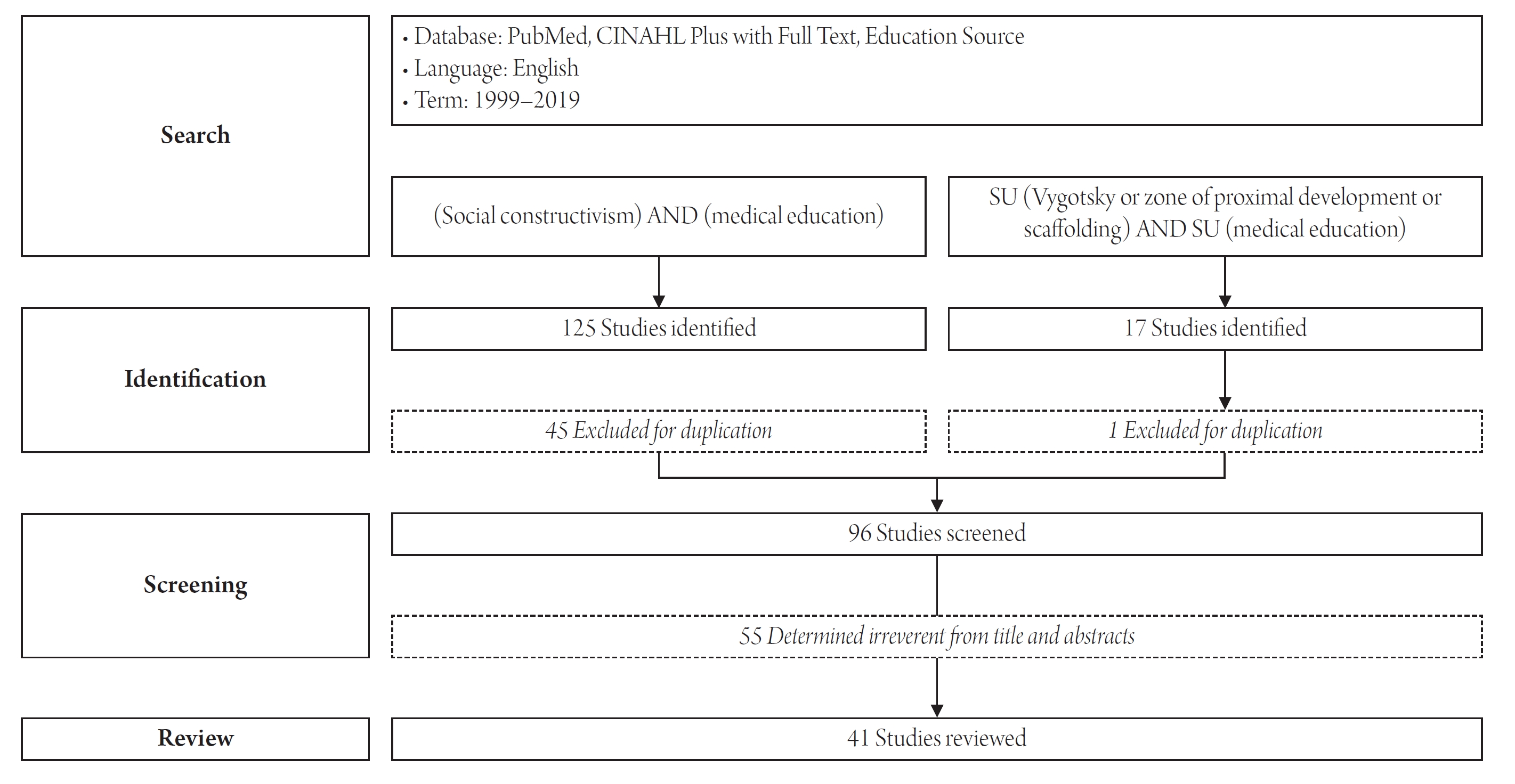
The purpose of this study is to discuss the main principles and concepts of social constructivism, examine the literature on the application of social constructivism in medical education, and explore the meaning and limitations of the utilization of social constructivism with learning theory. A literature search was carried out in two stages, utilizing PubMed, CINAHL and Education Source databases. The primary search included both fields (social constructivism AND medical education), while the secondary search was performed by subject (Vygotsky or ZPD or zone of proximal development or scaffolding AND medical education). A total of 96 papers were found through the primary and secondary searches, and after reviewing the abstracts of all 96 papers, 41 papers were deemed suitable for research purposes. In medical education, social constructivism is applied in areas such as (1) social and cultural behaviors (hidden curriculum), (2) social construct of “meaning” (dialogue and discourse), (3) learner’s identity transformation (expert), and (4) instructional intervention (ZPD and scaffolding). Social constructivism has provided many ideas to explore in terms of the composition of knowledge in the sociocultural context of health care, but it has not demonstrated an explicit instructional method or educational effects.
Social constructivism is an epistemology that explores the nature of knowledge—what it is and how it is formed and acquired [1-3]. Constructivism denies the notion of objective, universal knowledge or information and emphasizes the relativity of knowledge, highlighting the construction of knowledge by each individual in social, cultural, and historical contexts. However, constructivist thought was later critiqued for its failure to adequately consider the social context, as it took a radical turn towards the relativity of knowledge [3]. In response, constructivism evolved to incorporate Vygotsky’s perspective, which underscores the significance of social interaction and sociocultural factors. This led to a bifurcation into cognitive constructivism, which focuses on the construction of meaning through subjective experience, and social constructivism, which emphasizes the role of interaction within a sociocultural framework [2].
Social constructivism does not inherently explain learning phenomena [4]. Nevertheless, in the context of education, it is also used as a learning theory because it offers insights into various sociocultural factors from a learner-centered constructivist viewpoint. In the field of medical education, social constructivism has primarily served as a foundational theory for specific learning principles or teaching strategies [5-7], or as a supporting theory to advocate for the introduction and application of educational systems or policies [8-10]. From a methodological standpoint in medical research, the focus has been on language and relationships as they pertain to learner interactions. This includes investigating the content and processes of construction through the analysis of everyday life [11,12], the construction of meaning through experiences of community participation [13], and the process of identity formation as a physician in clinical practice [14-16]. Since the 2000s, research has also explored sociocultural factors, such as the sense of community within medicine [13], professionalism [17], interprofessional education [18,19], and international exchange [20].
This study examines the main concepts and principles of social constructivism and considers their implications for application in medical education. We will analyze the application of social constructivism’s concepts and principles within the realm of medical education and discuss how its epistemological framework can inform future learning theories.
The databases used for the literature search were PubMed (Medline), CINAHL (Cumulative Index to Nursing and Allied Health Literature), and Education Source (Figure 1). The search was limited to English-language studies and was conducted in two rounds with distinct purposes. The primary search aimed to identify how the epistemology of social constructivism is understood in the context of medical education. In the databases mentioned above, we searched for (social constructivism or social constructionist or social constructivist) AND (medical education or medical school or medical students or medical curriculum or medical student education or clinical education) as a full-text search.
The secondary search sought to identify how key concepts of social constructivism are applied to medical education. The same databases were searched using keywords (Vygotsky or ZPD or zone of proximal development or scaffolding) AND (medical education or medical school or medical students or medical curriculum or medical student education or clinical education). The primary search yielded 125 hits, and after excluding duplicates, 80 articles were identified. The secondary search identified 17 articles, excluding one duplicate article. The authors identified 96 abstracts and reviewed 41 studies, excluding those that (1) focused on disease treatment or patient education; (2) included gender, race, or interpretivist research; or (3) were more closely aligned with constructivist cognitive theory. To further explore the Korean context, we used RISS (Korea Education and Research Information Service) to search for the keywords “social constructivism <AND> education” and KoreaMed to search for the keywords “social constructivist Vygotsky or ZPD or zone of proximal development or scaffolding or social constructivist,” but no articles were identified.
Medicine is often viewed as a branch of sociology or social science. Scholars advocating for a social perspective on medicine have pointed to the insufficient emphasis on society or community engagement within medical education as a contributing factor to contemporary challenges in healthcare quality, health policy, and population health [21].
According to social constructivists, society is what sets humans apart from animals. As humans grow up, they assimilate the distinctive cognitive frameworks and behavioral patterns of their respective societies or communities [22]. Interactions with the community and its members are how an individual grows and develops. An individual’s interpretation of their society shapes social reality, while the collective understanding among community members establishes norms, identities, and institutions [23]. To participate in social life as a group member, one must internalize the culture—a historical construct—and live in accordance with the culture’s inherent values and behavioral expectations [23]. Society, in turn, is shaped by the traits of individuals that are forged within sociocultural relationships, leading to changes within the group. The cultural evolution of a society can be categorized into the social phase, which involves interaction with other members, and the internal psychological phase, which pertains to the individual [24].
Vygotsky’s theory of developmental psychology explains individual development in psychodynamic terms. While his research primarily addresses child development, the principles he outlines are equally applicable to the psychodynamic processes of adult learners in medical education. According to Vygotsky, learning is the internalization of cognitive development and functioning, facilitated by social interaction. Learners assess their societal roles, react to continuous social demands, and reframe their understanding and experiences. The active interpretation and re-interpretation inherent in this process culminate in learning [24].
According to Vygotsky [25], good learning is that which precedes development. The concept of the zone of proximal development describes how knowledge is constructed through the learning process and social participation [25]. This zone represents the gap between the actual and potential levels of development. The actual level of development is the stage at which the learner can solve problems independently, without assistance from others. In contrast, the potential developmental level indicates what the learner is capable of achieving with expert help.
Learners who begin as novices are progressively assigned a broader spectrum of tasks and responsibilities within the framework of continuous dialogue and interaction in social relationships [2,7]. The relationship between the novice and the expert begins with an unbalanced power dynamic. However, as the learner engages and evolves, their identity transforms, leading to the establishment of a new power structure [2]. The expert teaching methods used in this process include role modeling, feedback, questioning, teaching method, and cognitive structuring.
The concept of Vygotsky’s learning process was introduced by researchers aiming to pinpoint the key components of individualized instruction and was later refined to include the notion of scaffolding [26]. Scaffolding represents a type of social interaction between learners and instructors that facilitates the internalization of knowledge or skills. Instructor scaffolding serves as a mechanism to diminish the uncertainty inherent in the learning process, thereby broadening the potential for growth. Those who assist learners can be peers or experts in the subject matter. Rather than directly transferring knowledge, they function as guides or advisors.
The representative learning models that embody the theory of social constructivism in medical education are experiential learning and situational learning. The concept of experiential learning was formulated by integrating the social aspect of learning, as advocated by Vygotsky, into Piaget’s theory of experiential learning [5,6]. According to Kolb, who first developed the framework of experiential learning theory, learning is the process of creating knowledge through the transformation of experience [27]. In Kolb’s experiential learning theoretical framework, “experiential” or “informal” learning refers to new experiences that learners encounter in the work environment, often in an ambiguous and unstructured way. Through reflective observation of concrete experiences, learners form abstract conceptualizations of their learning. This conceptualized knowledge then advances to the stage of learning through active experimentation and application in real-life situations [28]. Experiential learning views the work environment as a learning space and translates experiences into learning with the guidance of a facilitator. This aligns with the core epistemology of knowledge acquisition in social constructivism, which emphasizes society, social interactions, and facilitation by instructors [27].
Situated learning posits that learning and development occur within a sociocultural context, transforming the learner through active participation in community activities. Initially, learners engage at the community’s periphery, interacting with and gradually integrating into the group, eventually taking on more central roles [28]. The cornerstone of situated learning is social interaction [7]. While the application of situated learning varies with context, in medical education, it effectively describes how novices evolve into competent practitioners. Novices are taught to recognize what to observe, understand how to interpret their observations, and learn how to communicate with colleagues and medical service providers within a community or social system that facilitates learning [7]. Consequently, the instructional design of situated learning focuses on creating the right context, scaffolding tasks between novices and experts, providing instructor coaching, and fostering learner interaction within the learning environment [7].
The following is an example of social constructivism applied to a physiology class. Teams are organized with consideration for the diverse backgrounds of learners. Authentic learning tasks are established, and student assessments are designed to reflect the dynamic interaction between the instructor and learners, as well as the progression of the learning experience [29].
Students form teams of five to six members. Each team is thoughtfully composed, considering various factors such as the students’ levels of experience, gender, age, and social backgrounds. As they study physiology, each team reflects on their own physiological processes—how biological principles manifest in their daily lives—and identifies three challenges they wish to prioritize during the course. Outside of regular class hours, student groups convene to define their roles. Instructors establish critical milestones to oversee the teams’ progress on their projects, offering feedback on the students’ objectives, experimental designs, and data interpretation. The groups carry out their experiments and are assessed based on their collaborative report writing and group presentations. The final product will include an analysis of the experimental design process, the implementation of the plan, the physiological interpretation of the results, and the limitations of the design. Approximately 10% of the final grade is allocated to self-assessment and peer assessment, evaluating teamwork, professionalism, and teammate feedback.
The preceding example illustrates how the core concepts of social constructivism can be adapted for classroom use. While the specific implementation may differ based on the objectives, subject matter, and audience of the educational program, this example offers practical insights into incorporating the fundamental principles of social constructivism into instructional design. Notably, the practice of reflecting on physiology (biological principles) plays a crucial role in facilitating development and learning through instructor-led intervention, or scaffolding, within each learner's zone of proximal development.
The application of a social constructionist perspective as a teaching and learning principle in medical education carries several important implications. First, it emphasizes social and cultural learning experiences. The aim of social constructivist learning is to facilitate an individual’s social integration and fit. Knowledge is not simply discovered; it is actively created within the social and cultural context to which one belongs. In medical education, the knowledge that learners construct is shaped by the situational, social, and cultural factors of medicine and healthcare. Therefore, it is essential to provide realistic, contextual, and field-based learning experiences that learners are likely to encounter or perform in practice [3,7,27]. Second, scaffolding is established within the zone of proximal development. Assistance tailored to the individual learner's zone of proximal development is meaningful. Even within the same environment, students have varying levels and backgrounds and can reach different levels of achievement with support. Moreover, the construction of learners’ knowledge is heavily influenced by their pre-existing knowledge systems [30]. Effective teaching interventions ensure that the level of achievement with assistance surpasses what learners could achieve on their own. Here, the instructor’s adaptive scaffolding for each learner aids in the internalization of knowledge or skills through social interactions between the learner and the instructor. Third, continuous interaction is crucial. Social interaction is the most significant factor in constructing learners’ understanding and meaning [30]. It provides opportunities to engage with learning experiences and is a means to construct one’s own knowledge by internalizing these experiences. In medical education, learners adopt the cultural behaviors of the existing community through sociocultural interaction and internalize their experiences by reflecting on them through interactions with experts or peers within the same community. Lastly, there is the growth of expertise. The zone of proximal development is not static; it is a dynamic area that evolves through continuous experience and reflection. In medical education, novices develop expertise by receiving guidance from experts within the zone of proximal development through legitimate peripheral participation [7]. Over time, learners who start as novices can evolve into responsible medical professionals capable of achieving expertise independently, without the need for expert assistance.
One theory cannot explain all situations in medical education learning. Moreover, because social constructivism does not explain learning phenomena, it does not inherently have implications for teaching methods. Colliver [4] argues that constructivism is ill-suited as a theory for teaching and learning, lacking practical utility in the context of medical education. The metaphorical language employed to describe phenomena within constructivist theory is fundamentally figurative and fails to provide sufficient prescriptive guidance to address challenges in teaching and learning.
Another issue with social constructivism in education is the ambiguous distinction between epistemology and the process of learning [1,4]. Social constructivism is often invoked as a principle that can explain the learning process, but the concept or principle actually implemented in educational contexts is either the construction of knowledge from a constructivist viewpoint or the acquisition of knowledge from an objectivist stance. Regardless of the approach adopted, most things will undergo significant changes [4]. Indeed, within the realm of medicine, which relies on generalized and formalized scientific knowledge, a constructivist teaching method that highlights the relativity of knowledge is merely one approach, suitable only for specific educational stages and content areas.
The theory of social constructivism in learning and development has served as a foundational framework for numerous experiments and research projects conducted by medical education scholars. It offers concepts that underpin both basic and applied research, potentially leading to the development of further theories. While social constructivism is not a standalone learning theory, it shares commonalities with various other learning theories and models. The theories, models, or strategies derived from social constructivism can be effectively implemented in educational settings.
One aspect of social constructivism theory that is particularly relevant to medical education is the sociocultural assimilation of individuals within a community. As individuals engage in dialogue with their peers, they exchange ideas and thoughts within a specific context [2,3]. In such scenarios, diverse structures of understanding may be assimilated, or cultural reproduction may occur through processes of shared participation and negotiation with others. During these interactions, the learner assumes the role of an interpreter of new information and becomes an “active co-constructor of meaning.”
Educational interest encompasses what learners encounter and assimilate upon joining the community. It pertains to the social and cultural elements within the medical community that learners are implicitly taught—or not taught—through a hidden curriculum, an unstructured and unintended educational layer [31]. Doja et al. [32] conducted interviews with members of the medical community and uncovered that students are being subtly indoctrinated with (1) the “privileges of experts in certain fields,” (2) the “reinforcement of hierarchy within the medical community,” and (3) a “culture of mutual tolerance for non-specialized content” as part of this hidden curriculum. Bryden et al. [33] observed that medical school faculty members recognized a discrepancy between their intended educational professionalism and their actual interactions with students, leading to feelings of inadequacy and failure in their inability to act as effective role models. Furthermore, studies have explored the perception and experience of unprofessional behaviors by healthcare providers or students—behaviors to which students are primarily exposed during clinical practice [34-36]. Research has also investigated the failure and fear of reporting medical errors [37], and educational approaches to address these issues through challenging their internalization [33,38,39].
Social constructivism deals with the nature of reality and how we come to know it [1]. It is characterized as a theoretical framework, meta-theory, or social theory. Within medical education, it emphasizes the interpretation of meanings that are created and shared in social and cultural contexts, as well as the experiences of individuals within the social structures upheld by these meanings [40]. Rees et al. [1] categorize the application of social constructivism theory in medical research into two categories: micro-constructivism and macro-constructivism. Micro-constructivism examines the everyday conversations that occur during social interactions, whereas macro-constructivism investigates the generative power of language in shaping social structures, relationships, and the influence of educational institutions. Rees et al. [11] explored the dynamics of power in the student-patient-doctor relationship by analyzing video or audio recordings of interactions at the bedside during clinical training in a hospital. They focused on the social processes at play. Another study analyzed the structure of everyday conversations by examining reflective conversations among a group of medical students [12]. The findings indicated that despite individual differences, all participants consistently engaged in activities such as identifying meaningful events, discussing reasons for sharing, addressing learning issues, and participating in learning. Research on discourse within the social organization of medical schools includes an investigation into the identity formation of Canadian medical students with disabilities. Stergiopoulos et al. [41] analyzed data from student interviews, institutional documents, and student blogs at cultural, social, and relational levels. Their research aimed to understand how medical students with disabilities construct their identities. They uncovered potential curricular content and examined how students defined the concepts of a “good student” and a “good patient,” as well as the idea of wellness within the context of developing an identity that encompasses “my disability” and becoming “professionals who must objectify disability.”
One of the key principles in social constructivism is the evolution of the learner’s role within the zone of proximal development. Initially, learners take a passive role, following the guidance of a mentor. However, they transition to an active role as they engage in problem-solving. Through this process, they not only rely on their newly acquired knowledge but also develop cognitive strategies for transferring this knowledge. They learn new concepts and apply them to novel situations. In the realm of professional development in medicine, this shift in the learner’s role is often equated with professional growth. Medical education views the learner as both a social and institutional entity, evolving from a peripheral participant to a core member of the medical community [42]. A transformation of identity from novice to expert is expected as students continue to participate in the community and broaden their participation through the experience of solving tasks in real-world situations with an expert instructor [43]. Hansen et al. [44] applied the social constructivist framework to explore the process of identity transformation among family medicine physicians. By comparing three cohorts—before, during, and after family medicine residency training—over approximately 12 years, they documented the broadening of expertise. This progression saw family physicians move from being under the tutelage of supervising physicians to treating patients independently, and eventually to conducting research in family medicine. The study highlighted that the experiences of the learner and the influence of role models are pivotal in shaping the identity of a specialist physician.
Another debate related to professional identity formation revolves around the conflict between the diversity of physician identities and the standardization that medical education promotes. According to Frost and Regehr [14], diversity in identity formation involves individualization, difference, and multiple possibilities, suggesting that heterogeneity is beneficial to medical education and patients. In contrast, the argument for standardization centers on uniformity, similarity, and restricting possibilities to establish a single way of being a competent and professional physician. The authors propose leveraging the conflicting and contentious contexts of these discourses to shape the professional identity of medical students.
Learners in medical education often identify learning challenges when they encounter unfamiliar rules or contexts. In such instances, the instructor’s role is to facilitate the learning process as a guide, rather than merely transmitting knowledge [30].
The concept of social constructivism’s zone of proximal development and scaffolding in learning situations is more akin to a metaphorical expression of phenomena than concrete teaching and learning methods. Since metaphorical expressions do not constitute explicit tools or methods in themselves, it is challenging to standardize their application in experimental or practical contexts. Consequently, much of the research on the development and effectiveness of teaching methods within medical education has been confined to the creation of web-based support tools. These tools include features such as instructor advice or pre-set “help” options for learners who encounter difficulties in digital learning environments [45-47]. In the field of medicine, these concepts have primarily been applied to the learning process that leads to a medical diagnosis. The scaffolding methods identified include visual or conceptual hinting [46], the presentation of representative cases [48], and cognitive activation through questioning [49]. Mixed results have been reported for the effectiveness of the training, with some studies showing that providing appropriate representations of the diagnostic process through medical reasoning increased the efficiency of subsequent diagnoses [48] and others showing no significant difference in the virtual environment compared to other comparison groups [47].
The application of social constructivism in medical education varies widely in scope and content. It includes analyzing learners’ discourse to focus on the construction of meaning, employing it as a foundational theory to explain specific models or principles of learning, and using metaphorical expressions of development and learning as a strategy for teaching in medical education. The sporadic application of this theory across different contexts indicates that social constructivism has not been definitively established as a learning theory in this field.
Social constructivism offers a framework for understanding the nature of knowledge and the process by which it is constructed. To effectively employ knowledge and knowledge formation as theories of learning, it is necessary to establish clear principles that define the core concepts and their significance within various aspects of education or learning. These principles can then be implemented in practical settings, where their value and efficacy can be demonstrated through a process of development and application. Despite its potential, the application of social constructivism in medical education has largely been confined to the learning process. It serves as a foundation for endorsing specific policies or content, or as a valued learning theory within certain contexts of medical education. However, there are challenges in discerning the specific role it plays within the context of medical education and in distinguishing the educational outcomes it generates from those produced by other learning theories.
From a sociocultural perspective, social constructivism plays a significant role in understanding how individual learners construct and apply knowledge within a social context. In the realm of medical education, social constructivism does not refute the existence of objective entities or knowledge. Instead, it highlights the importance of constructing meaning as individuals with diverse backgrounds and experiences engage with one another to exchange and develop distinct interpretations. These concepts are effectively used to investigate the culture and society of healthcare, encompassing aspects such as knowledge and identity.
The discourse on social constructivism has significantly influenced the field of education, inspiring a multitude of ideas. This discourse has broadened its reach across various disciplines, and its principles have become so widely accepted that they are often assumed in the design and experimentation of educational settings without explicit reference to the underlying theory. However, this study is constrained by its methodological approach—namely, a literature review that specifically searched for terms such as “social constructivism,” “Vygotskian,” “zone of proximal development,” or “scaffolding.” Consequently, studies that did not explicitly mention these terms were not included in the review.
In the field of education, even when social constructivism is not explicitly mentioned, the objectives of education, as well as the processes of teaching and learning, and their evaluation, are often developed and implemented based on a widely accepted epistemology. To analyze and apply social constructivism in medical education more practically and effectively, additional research is necessary to identify and examine potential applications. We recommend further investigation into how social constructivist epistemology is manifested in various educational domains, which factors are deemed critical in the transition from epistemology to teaching and learning theory, and which instructional design principles are essential for optimizing educational outcomes.
NOTES
REFERENCES
1. Rees CE, Crampton PE, Monrouxe LV. Re-visioning academic medicine through a constructionist lens. Acad Med. 2020;95(6):846-50. https://doi.org/10.1097/ACM.0000000000003109


2. Kang I. A brief reflection on cognitive and social constructivism. Korean J Educ Technol. 1995;11(2):48-63. https://doi.org/10.17232/KSET.11.2.3

3. Cobb P, Yackel E. Constructivist, emergent, and sociocultural perspectives in the context of developmental research. Educ Psychol. 1996;31(3-4):175-90. https://doi.org/10.1080/00461520.1996.9653265

4. Colliver JA. Constructivism: the view of knowledge that ended philosophy or a theory of learning and instruction? Teach Learn Med. 2002;14(1):49-51. https://doi.org/10.1207/S15328015TLM1401_11


5. Kolb AY, Kolb DA. Learning styles and learning spaces: enhancing experiential learning in higher education. Acad Manag Learn Educ. 2005;4(2):193-212. https://doi.org/10.5465/amle.2005.17268566

6. Dennick R. Constructivism: reflections on twenty five years teaching the constructivist approach in medical education. Int J Med Educ. 2016;7:200-5. https://doi.org/10.5116/ijme.5763.de11



7. Brown JS, Collins A, Duguid P. Situated cognition and the culture of learning. Educ Res. 1989;18(1):32-42. https://doi.org/10.3102/0013189X018001032

8. Hirshfield LE, Underman K. Empathy in medical education: a case for social construction. Patient Educ Couns. 2017;100(4):785-7. https://doi.org/10.1016/j.pec.2016.10.027


9. Hamdy H. Medical college of the future: from informative to transformative. Med Teach. 2018;40(10):986-9. https://doi.org/10.1080/0142159X.2018.1498628


10. Philpott J, Batty H. Learning best together: social constructivism and global partnerships in medical education. Med Educ. 2009;43(9):923-4. https://doi.org/10.1111/j.1365-2923.2009.03436.x


11. Rees CE, Ajjawi R, Monrouxe LV. The construction of power in family medicine bedside teaching: a video observation study. Med Educ. 2013;47(2):154-65. https://doi.org/10.1111/medu.12055


12. Veen M, de la Croix A. The swamplands of reflection: using conversation analysis to reveal the architecture of group reflection sessions. Med Educ. 2017;51(3):324-36. https://doi.org/10.1111/medu.13154


13. Dube T, Schinke R, Strasser R. It takes a community to train a future physician: social support experienced by medical students during a community-engaged longitudinal integrated clerkship. Can Med Educ J. 2019;10(3):e5-16. https://doi.org/10.36834/cmej.43460

14. Frost HD, Regehr G. “I am a doctor”: negotiating the discourses of standardization and diversity in professional identity construction. Acad Med. 2013;88(10):1570-7. https://doi.org/10.1097/ACM.0b013e3182a34b05


15. Gordon LJ, Rees CE, Ker JS, Cleland J. Dimensions, discourses and differences: trainees conceptualising health care leadership and followership. Med Educ. 2015;49(12):1248-62. https://doi.org/10.1111/medu.12832


16. Van der Zwet J, Zwietering PJ, Teunissen PW, van der Vleuten CP, Scherpbier AJ. Workplace learning from a socio-cultural perspective: creating developmental space during the general practice clerkship. Adv Health Sci Educ Theory Pract. 2011;16(3):359-73. https://doi.org/10.1007/s10459-010-9268-x



17. Gleeson C. Education beyond competencies: a participative approach to professional development. Med Educ. 2010;44(4):404-11. https://doi.org/10.1111/j.1365-2923.2009.03601.x


18. Andrews T. What is social constructionism? Grounded Theory Rev. 2012;11(1):39-46.
19. Ritchie C, Gum L, Brewer M, Sheehan D, Burley M, Saunders-Battersby S, et al. Interprofessional collaborative practice across Australasia: an emergent and effective community of practice. Focus Health Prof Educ Multi-Discip J. 2013;14(2):71-80.
20. Jacobs F, Stegmann K, Siebeck M. Promoting medical competencies through international exchange programs: benefits on communication and effective doctor-patient relationships. BMC Med Educ. 2014;14:43. https://doi.org/10.1186/1472-6920-14-43



21. Sales CS, Schlaff AL. Reforming medical education: a review and synthesis of five critiques of medical practice. Soc Sci Med. 2010;70(11):1665-8. https://doi.org/10.1016/j.socscimed.2010.02.018


22. Russell DR. Vygotsky, Dewey, and externalism: beyond the student/discipline dichotomy. J Adv Compos. 1993;13(1):173-97.
23. Shin J. Implications of social constructivism on special education: focusing on Vygotsky’s defectology. Asian J Educ. 2001;2(1):37-54.
24. Rieber RW, Carton AS. Emotions and their development in childhood. In: Rieber RW, Carton AS, editors. The collected works of L. S. Vygotsky: problems of general psychology, including the volume thinking and speech. New York (NY): Springer; 1987. p. 325-37.
25. Vygotsky LS. Tool and symbol in child development. In: Cole M, Jolm-Steiner V, Scribner S, Souberman E, editors. Mind in society: development of higher psychological processes. Cambridge (MA): Harvard University Press; 1978. p. 19-31.
26. Wood D, Bruner JS, Ross G. The role of tutoring in problem solving. J Child Psychol Psychiatry. 1976;17(2):89-100. https://doi.org/10.1111/j.1469-7610.1976.tb00381.x


27. Yardley S, Teunissen PW, Dornan T. Experiential learning: AMEE guide no. 63. Med Teach. 2012;34(2):e102-15. https://doi.org/10.3109/0142159X.2012.650741


28. Kaufman D, Mann KV. Teaching and learning in medical education: how theory can inform practice. In: Swanwick T, editor. Understanding medical education: evidence, theory and practice. 2nd ed. Chichester: Wiley-Blackwell; 2014. p. 7-29.
29. Kay D, Kibble J. Learning theories 101: application to everyday teaching and scholarship. Adv Physiol Educ. 2016;40(1):17-25. https://doi.org/10.1152/advan.00132.2015


30. Cantillon P. Becoming a better teacher. In: Cantillon P, Wood DF, Yardley S, editors. ABC of learning and teaching in medicine. 3rd ed. Hoboken (NJ): John Wiley & Sons; 2017. p. 1-2.
31. Mahood SC. Medical education: beware the hidden curriculum. Can Fam Physician. 2011;57(9):983-5.


32. Doja A, Bould MD, Clarkin C, Eady K, Sutherland S, Writer H. The hidden and informal curriculum across the continuum of training: a cross-sectional qualitative study. Med Teach. 2016 Apr;38(4):410-8. https://doi.org/10.3109/0142159X.2015.1073241

33. Bryden P, Ginsburg S, Kurabi B, Ahmed N. Professing professionalism: are we our own worst enemy?: faculty members’ experiences of teaching and evaluating professionalism in medical education at one school. Acad Med. 2010;85(6):1025-34. https://doi.org/10.1097/ACM.0b013e3181ce64ae


34. Binder R, Friedli A, Fuentes-Afflick E. Preventing and managing unprofessionalism in medical school faculties. Acad Med. 2015;90(4):442-6. https://doi.org/10.1097/ACM.0000000000000592


35. Reddy ST, Farnan JM, Yoon JD, Leo T, Upadhyay GA, Humphrey HJ, et al. Third-year medical students’ participation in and perceptions of unprofessional behaviors. Acad Med. 2007;82(10 Suppl):S35-9. https://doi.org/10.1097/ACM.0b013e3181405e1c


36. Spiwak R, Mullins M, Isaak C, Barakat S, Chateau D, Sareen J. Medical students’ and postgraduate residents’ observations of professionalism. Educ Health (Abingdon). 2014;27(2):193-9. https://doi.org/10.4103/1357-6283.143790


37. Lee SH, Shin YH, Kim SS. Comparing attitudes toward disclosing medical errors between medical students and interns. Korean J Med Educ. 2012;24(3):247-58. https://doi.org/10.3946/kjme.2012.24.3.247



38. Franco RS, Franco CA, Kusma SZ, Severo M, Ferreira MA. To participate or not participate in unprofessional behavior: is that the question? Med Teach. 2017;39(2):212-9. https://doi.org/10.1080/0142159X.2017.1266316


39. Welsh D, Zephyr D, Pfeifle AL, Carr DE, Fink JL 3rd, Jones M. Development of the barriers to error disclosure assessment tool. J Patient Saf. 2021;17(5):363-74. https://doi.org/10.1097/PTS.0000000000000331

40. Vall Castello B. Bridging constructivism and social constructionism: the journey from narrative to dialogical approaches and towards synchrony. J Psychother Integr. 2016;26(2):129-43. https://doi.org/10.1037/int0000025

41. Stergiopoulos E, Fernando O, Martimianakis MA. “Being on both sides”: Canadian medical students’ experiences with disability, the hidden curriculum, and professional identity construction. Acad Med. 2018;93(10):1550-9. https://doi.org/10.1097/ACM.0000000000002300


42. Maudsley G, Strivens J. Promoting professional knowledge, experiential learning and critical thinking for medical students. Med Educ. 2000;34(7):535-44. https://doi.org/10.1046/j.1365-2923.2000.00632.x


43. Collins A. Cognitive apprenticeship and instructional technology. In: Idol L, Jones BF, editors. Educational values and cognitive instruction: implications for reform. Hillsdale (NJ): Lawrence Erlbaum Associates, Inc.; 1991. p. 121-38.
44. Hansen SE, Mathieu SS, Biery N, Dostal J. The emergence of family medicine identity among first-year residents: a qualitative study. Fam Med. 2019;51(5):412-9. https://doi.org/10.22454/FamMed.2019.450912


45. McConnaughey S, Freeman R, Kim S, Sheehan F. Integrating scaffolding and deliberate practice into focused cardiac ultrasound training: a simulator curriculum. MedEdPORTAL. 2018;14:10671. https://doi.org/10.15766/mep_2374-8265.10671



46. Nivala M, Saljo R, Rystedt H, Kronqvist P, Lehtinen E. Using virtual microscopy to scaffold learning of pathology: a naturalistic experiment on the role of visual and conceptual cues. Instr Sci. 2012;40:799-811. https://doi.org/10.1007/s11251-012-9215-8

47. Braun LT, Borrmann KF, Lottspeich C, Heinrich DA, Kiesewetter J, Fischer MR, et al. Scaffolding clinical reasoning of medical students with virtual patients: effects on diagnostic accuracy, efficiency, and errors. Diagnosis (Berl). 2019;6(2):137-49. https://doi.org/10.1515/dx-2018-0090


48. Braun LT, Zottmann JM, Adolf C, Lottspeich C, Then C, Wirth S, et al. Representation scaffolds improve diagnostic efficiency in medical students. Med Educ. 2017;51(11):1118-26. https://doi.org/10.1111/medu.13355


49. Hmelo C, Day R. Contextualized questioning to scaffold learning from simulations. Comput Educ. 1999;32(2):151-64. https://doi.org/10.1016/S0360-1315(98)00062-1

-
METRICS

-
- 0 Crossref
- 0 Scopus
- 1,051 View
- 28 Download
- ORCID iDs
-
Youngjon Kim

https://orcid.org/0000-0002-0445-526X - Related articles
-
The 2024 Medical Crisis : Challenges for Medical Education2024 June;26(2)
Cognitive Constructivism in the Development of Medical Education2024 January;26(Suppl1)
Introduction to YouTube Channels Useful for Medical Education2023 October;25(3)


 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print


